I’ve just returned from the New Zealand Veterinary
Association’s first ever wellbeing symposium, held in Christchurch. I was
invited there to speak about ethics rounds, an intervention designed to help
veterinary team members with ethically challenging situations that can lead to
moral stress, moral distress, or even moral injury. More on that in a later
post.
The reason for today’s post is to share a couple of
the themes discussed at the symposium.
The MC, Dr Charlotte (Lotte) Cantley, opened the
symposium with an incredible account of her recovery following a catastrophic
and near fatal horse-riding accident (the horse was okay), and a grueling
schedule of treatment and rehabilitation. According to Lotte, “resilience is
not bouncing back to how we were but being flexible, adapting to and embracing
the uncomfortable changes life throws at us”.
Given her account, uncomfortable is an understatement.
So here is my take on the major themes of the first
day.
Collegiality and compassion
One thing that came through loud and clear was that
one of the biggest impediments to the wellbeing of veterinary team members is,
well, other veterinary team members. The way we treat one another, whether we
are aware of it or not, impacts us. As speaker after speaker raised this issue,
heads around the room nodded. Tears were quietly shed.
Sonja Olson, author of Creating Wellbeing and Building
Resilience in the Veterinary Profession, argued that we need to stop referring
to communication and people skills as “soft skills” and name them what they are
– power skills, tools that improve collegiality, understanding, shared decision
making, adherence to negotiated recommendations and ultimately, good clinical
and policy outcomes. https://www.routledge.com/Creating-Wellbeing-and-Building-Resilience-in-the-Veterinary-Profession/Olson/p/book/9780367418793
Dana Carver, from GoodYarn (an evidence-based,
peer-delivered mental health literacy program https://www.goodyarn.org/) , talked about situations that negatively
impact our mental health. As she said, when we suffer an obvious “sudden
negative change or event” (like the death of a family member), people tend to
be demonstrative in their care. They swoop in with offers of assistance. They
make casseroles. But what happens when we experience other things that
negatively impact our mental health? According to Dana, these include things
like a lack of justice, a lack of life balance, relationship problems, poor
physical health or chronic pain? In these situations, we aren’t good at asking
for help…and people may not offer it. What we can do is make time, or make an
effort to connect in some way. Its better to do something, ask the question,
say something, than worry about looking like an idiot. I could recall plenty of
missed opportunities to extend support to someone, to make that casserole.
We heard a lot about implementing wellbeing plans into
practice, and ensuring that this was more than just promoting a token day.
Stephen Hopkinson, the founder of a large dairy practice surveyed his own staff
to ensure that the wellbeing plan subsequently developed would actually meet
their needs. To his surprise, they found that gossip, negative comments,
exclusion and not helping others were the number 1 things negatively impacting
staff.
Sometimes this is coming from a place of anxiety or
hurt. Those behaving this way may not even be aware that they are having this
impact.
He argued that we need to ensure that the discussion
about mental wellbeing isn’t just about vets. All team members need
recognition. Hence his team celebrate:
- -
National Administrative Professionals
day (April 26)
- -
World Veterinary Day (April 30)
- -
National Receptionist day (10 May)
- -
Veterinary Nurse and Technician
Appreciation day (14 October)
Because winters are cold in New Zealand, they also run
“soup days” in winter – providing staff with a small budget to buy ingredients
on the practice account, so they can make soups and share with the team. According
to them, this marries well with the “5 Ways to Wellbeing”:
- Keep learning – learn a new soup recipe
- Be active – dance and sing when you make the soup
- Give – share the end product
- Take-notice – mindfully sip your soup
- Connect – rate each other’s soups, swap recipes, and cook together
Denise Quinlan, who acknowledged that everyone gets
crispy, shared her strategies:
- - Prioritise ruthlessly (so if someone asks you to do something new, which thing on your to do list do you need to bump?)
- -
Promote autonomy in the workplace
- -
Support one another
- -
Value each other
- -
Act fairly (avoid those perceived
injustices)
- -
Provide clarity (lack of clarity
about job roles was a big reason for people to be disgruntled at work)
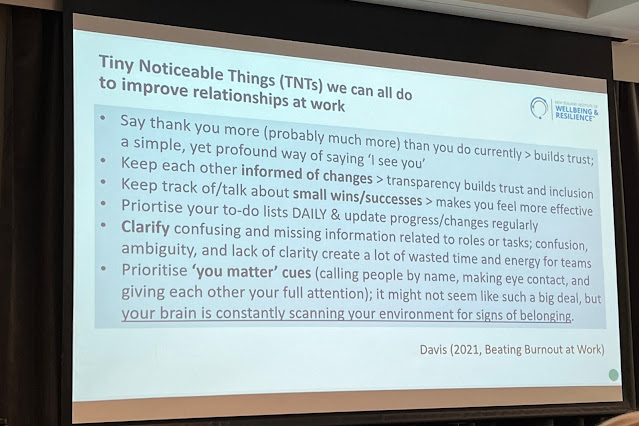
Her colleague, Paula Davis (author of Beating Burnout
at Work https://stressandresilience.com/burnout-book/
), provided a list of “Tiny Noticeable Things” that we can do at work to help
demonstrate that we value each other.
Source: Paula Davis, Beating Burnout at Work.
Imposter syndrome
Every speaker admitted that they have imposter syndrome.
In fact, Sonja has given hers a name (I won’t share it here, you’ll have to ask
her).
Imposter syndrome is well-documented among the general
population, as well as veterinary team members https://pubmed.ncbi.nlm.nih.gov/32571984/
. It tends to flare when we try something new, or perform in front of our
peers, or start a new job. In a profession where life and death and animal welfare and human wellbeing so often hang in the balance, imposter syndrome can
serve us well, driving us to improve, not to rest on our laurels. No one could
pin down a guaranteed way to manage imposter syndrome without throwing the baby
out with the bathwater…but it helps to know that imposter syndrome is something
that everyone struggles with – and probably gets worse the higher we achieve.
Massey University Dean of Veterinary Education Jenny
Weston did remind everyone that we can ultimately be our own worst colleagues –
engaging in critical, judgmental, and negative self-talk that we would never
extend to anyone else. Not only did she have everyone up on the dancefloor –
she commandeered a team of well-practiced back-up dancers.
Rather than worrying about our own imposter syndrome
(she/he/they are, realistically, probably not going to leave us – as per above,
they do serve us well on occasion), maybe it’s more productive to recognise
that others are experiencing this too, and be aware of the way we might impact
those around us by inadvertently reenforcing that, and perhaps not doing enough to show our appreciation.