|
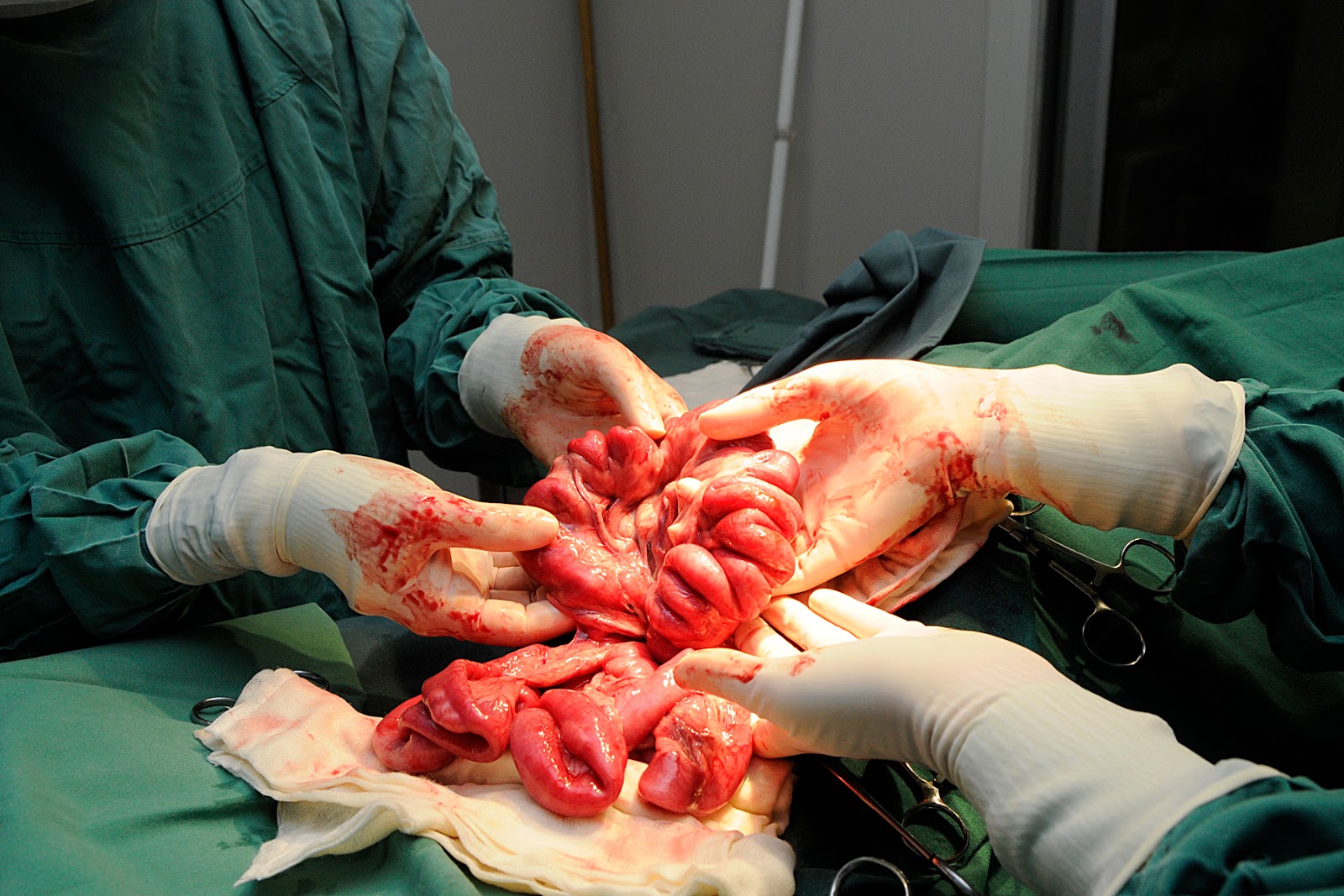
| How do you learn veterinary science well, and how on earth do you teach well, when there is so much information to wrestle with? |
As a lecturer I am frequently asked for study tips and
strategies by veterinary students. However, earlier this year I was informed by
one student that she had found the Holy Grail: a book entitled How to Study in Medical School by Armin
Kamyab.
I critiqued this book (read the post here) on the grounds that I felt it placed
far too much emphasis on memorising everything taught, leaving little room to
acquire experience in what is an overwhelmingly hands-on field.
Kamyab's system is based on several problematic assumptions, one of which is
that everything taught in the medical curriculum is worthy of equal
consideration, equal revision and hopefully absorption. Discipline, he argues,
is the answer.
But if we extend this to the veterinary curriculum, my own
experience tells me that discipline is not enough. What happens when we reach
capacity, or information overload?
In 1980 – well before the internet, social media and any
form of portable telecommunication – Anderson & Graham raised concerns
about the impact of information overload on medical education. They performed a
loose analysis of the amount of information taught in the medical curriculum
and determined that undergraduate medical students had to assimilate 27,000
facts and 25,500 concepts in their clinical or senior years (roughly 9 facts or
concepts per hour).
The authors concluded that there was a need to establish the
“best and most efficient means of transmitting and assimilating information”
(Anderson & Graham, 1980). That was 23 years ago. Surveys of veterinary
students at Murdoch University and the University of Queensland identified
information overload as a major stressor (Williams et al., 2005; McLennan & Sutton, 2005). But it isn’t just
undergraduates suffering under the weight of too much information (read the late Dr Lee Lipsenthal's arguments in this post).
Graduates, too, are struggling with the onslaught of new
research, new technologies, new techniques and aggressive marketing of
veterinary continuing education (every week there seems to be a new provider springing up somewhere).
 |
| An old tree near the Main Quad at the University of Sydney. |
According to some, the rate of information overload is no
longer relevant. Veterinary educators long ago recognised the inadequacies of
the traditional assumptions underpinning undergraduate teaching (Bushby, 1994,
see table 1).
Table 1. Rules defining traditional veterinary medical
education
|
Assumptions underpinning curriculum...
|
Problems with that assumption...
|
|
There is a core of information that must be learned.
|
No two teachers agree on the core;
The core is difficult to refine (one attempt resulted in a
program consisting of 216,000 objectives or one fact every six minutes
|
|
Teachers will tell the student what they must know.
|
Assumes that teachers know what needs to be learned;
Assumes students are passive, surface learners.
|
|
Teachers must cover the material.
|
If students don’t learn it is their fault; teachers are dissociated
from the learning process.
|
|
The teacher determines the organisation of material and
method of instruction.
|
The student plays no role in deciding how the material is
organised or learned.
|
|
With sufficient knowledge students will learn to think
|
Students do not feel in control of learning and are only
exposed to critical thinking late in the course.
|
|
The only valuable information is that which is stored in
your head.
|
Memorisation, superficial understanding and guessing are
rewarded; exploration, inquiry, thoroughness and reliability are penalised.
|
Adapted from Bushby (1994).
The argument against the traditional model is compelling,
yet my own experience as a veterinary undergraduate – and feedback from my
students – tells me that we have significant attachment to this model.
The most compelling evidence, to me, was interviewing students last semester as part of my Graduate Certificate in Educational Studies (if you're interested in this course visit here).
When I interviewed veterinary students last semester about
learning, 100 per cent stated that they had learned something when they had
memorised it. Not when they could explain it, no mention even
of applying that morsel of knowledge. On Saljo’s hierarchy of learning, these excellent students only reached the middle. And memorising something is far different from applying it.
One of my lecturers once said that "vet school is wasted on vet students", i.e. they don't have a context to hang those factoids they are learning, nor an appreciation of their relative importance, so it doesn't make sense til they graduate by which time they've forgotten a large proportion of said factoids. I got what he meant - but does it have to be that way? If we move away from the assumptions that to be a good vet you need to memorise every fact taught in vet school, and good veterinary teachers teach good veterinary facts, what are we left with?
[Sorry for the cliffhanger, but this is a topic I will be posting on further. I am genuinely keen to hear from students, veterinary educators and vets about their take on the problem - is it really a problem? How do you learn? What is a good teacher and how can we teach veterinary science best? Send me an email or post a comment].
References:
Anderson J and Graham A (1980) A problem in medical
education: is there an information overload? Medical Education 14:4-7.
Bushby P (1994) Tackling the knowledge explosion without
overloading the student. Australian
Veterinary Journal 71:372-374.
McLennan MW and Sutton RH (2005) Stress in veterinary
science students: a study at the University of Queensland. Journal of Veterinary Medical Education 32(2):213-218.
Trigwell K (2001) Judging university teaching. International Journal for Academic
Development 6:1, 65-73.
Viner B (2010) Success in Veterinary Practice: Maximising
Clinical Outcomes and Personal Well-Being. Oxford: Wiley & Sons.
Williams SM, Arnold PK, Mills JN (2005) Coping with stress:
a survey of Murdoch University Veterinary Students.